Hyponatremia In Liver Disease
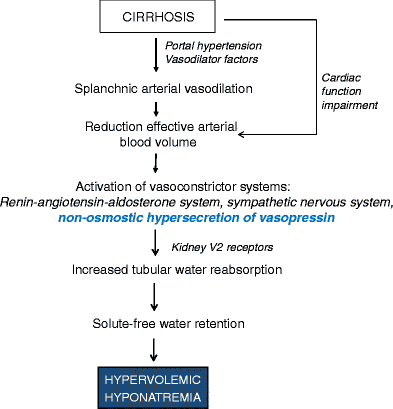
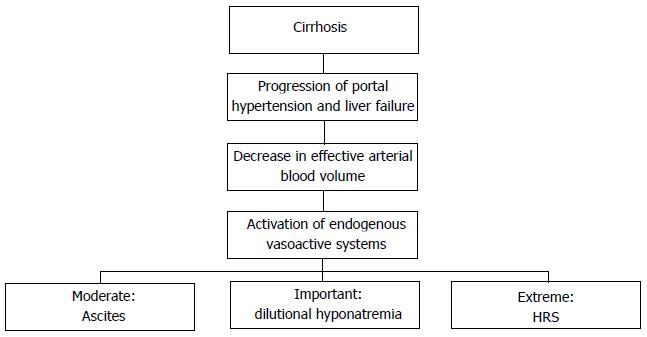
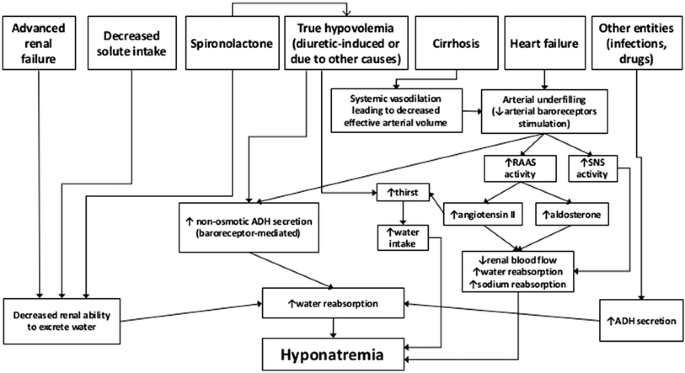
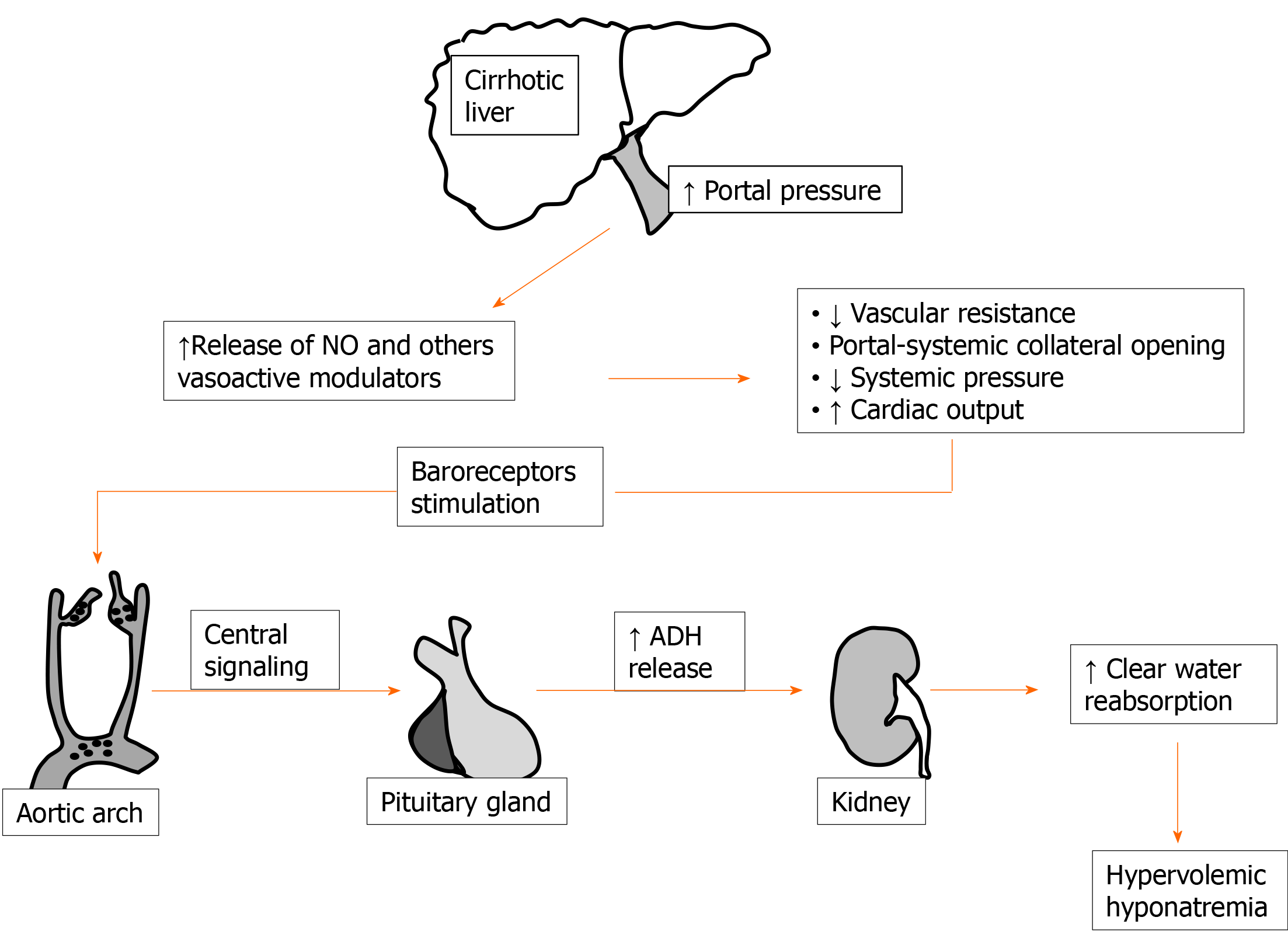
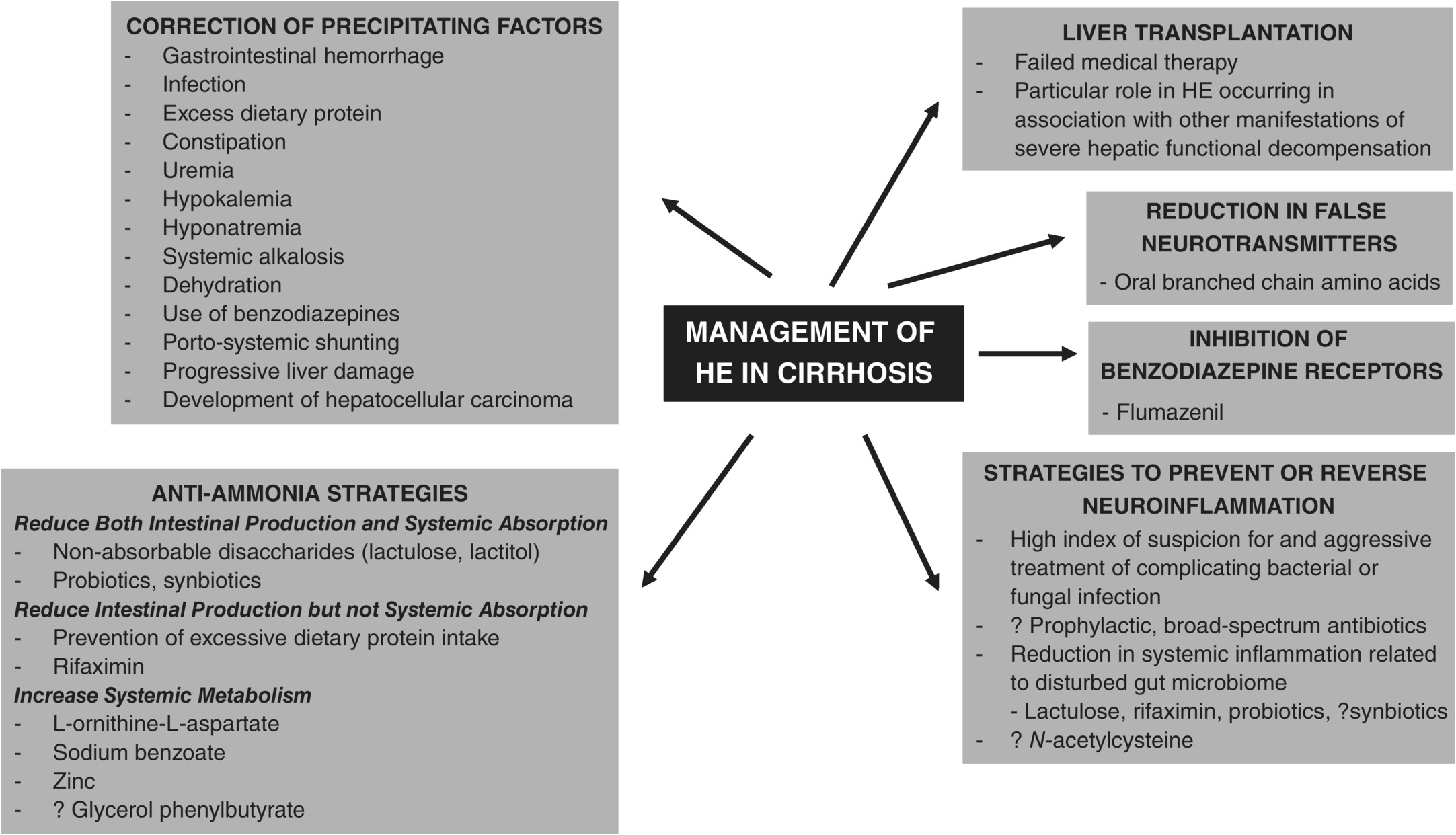
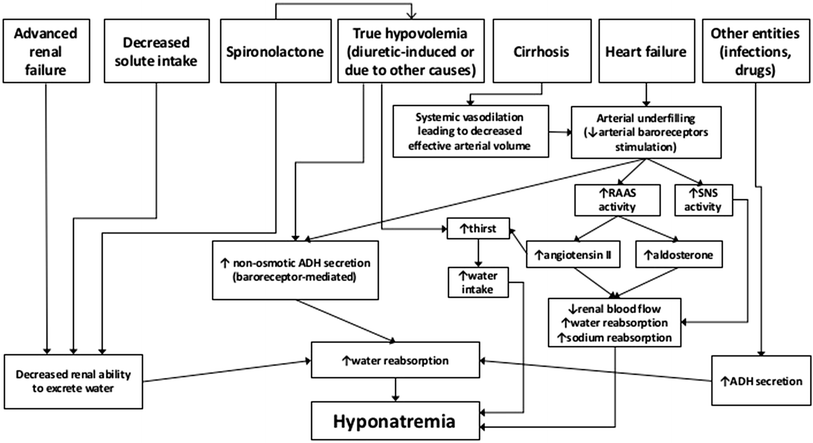
Hyponatremia in liver disease. Hyponatremia is also associated with numerous complications in liver disease patients including severe ascites hepatic encephalopathy infectious complications renal impairment increased severity of liver disease in cirrhosis and increased hospital stay and neurologicinfectious complications posttransplant. The pathogenesis of hyponatremia in these patients is directly related to the hemodynamic changes and secondary. Liver transplantation is the only definitive treatment for end stage liver diseases.
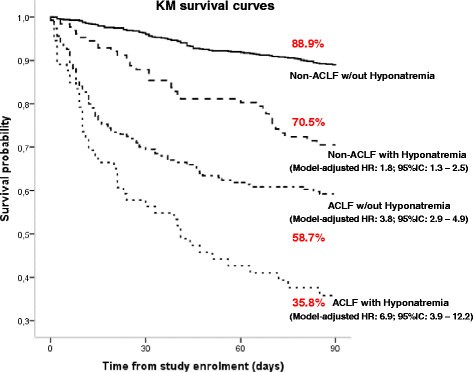
Furthermore hyponatremia and renal dysfunction are associated with poor prognosis. Asymptomatic hyponatremia is not recommended. The pathophysiology of hyponatremia in cirrhosis is complex and multifactorial.
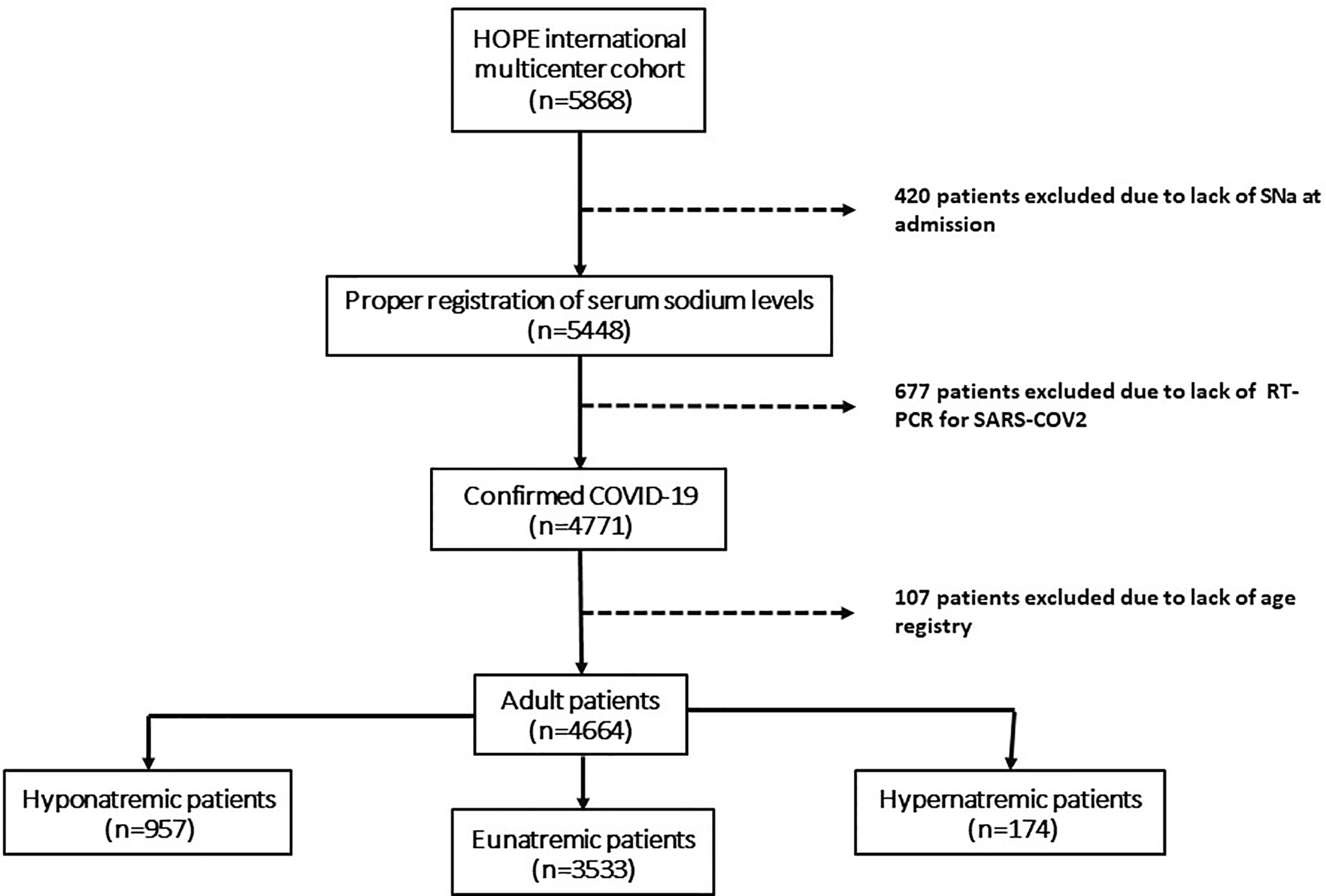
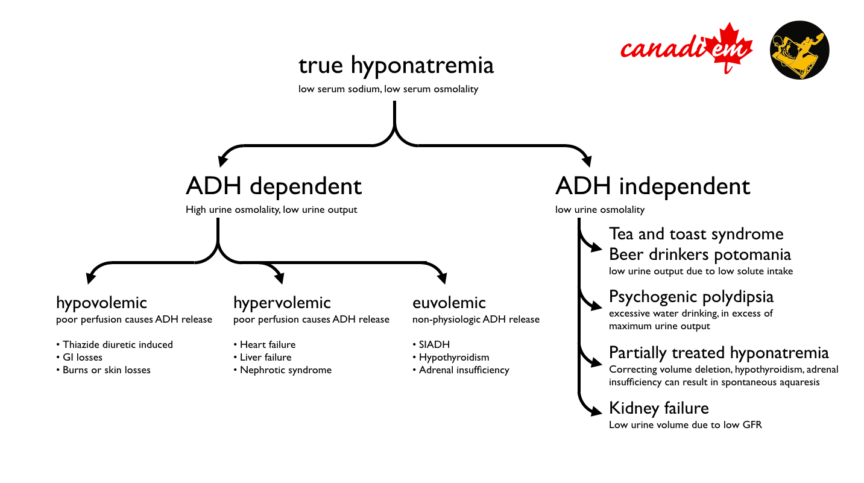
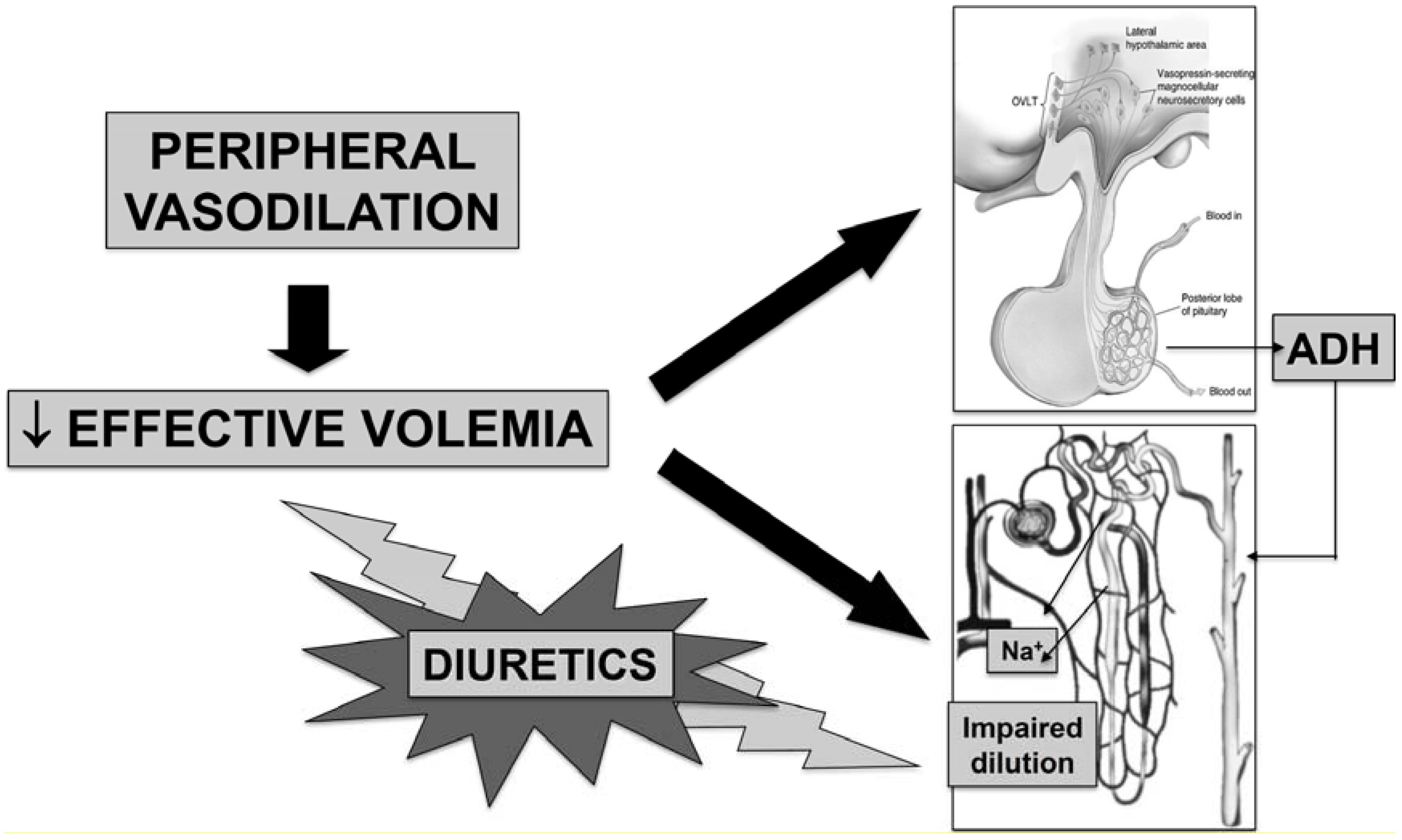
Tolvaptan is not recommended in patients with liver disease. In patients without liver disease hyponatremia is primarily associated with a broad variety of neurological manifestations related to the existence of brain edema such as headache disorientation confusion focal neurological deficits seizures and in some cases death due to cerebral herniation. It usually develops in those with refractory ascites and is a manifestation of the nonosmotic release of arginine vasopressin AVP.
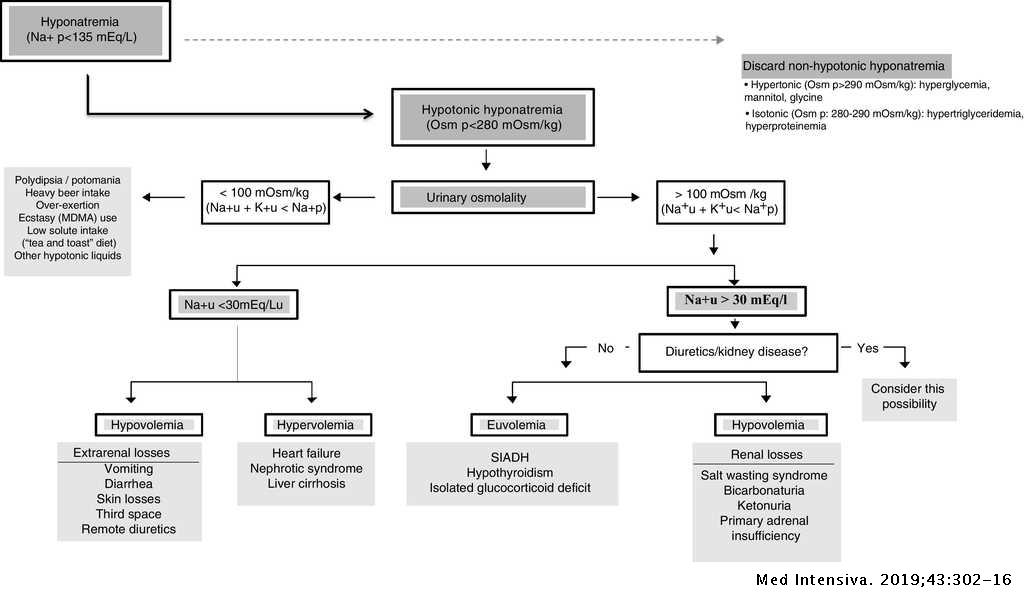
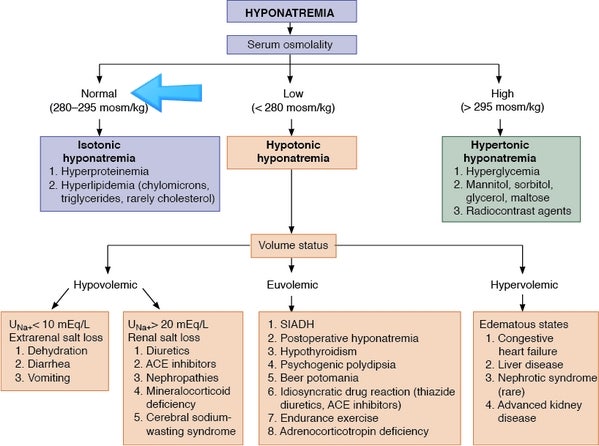
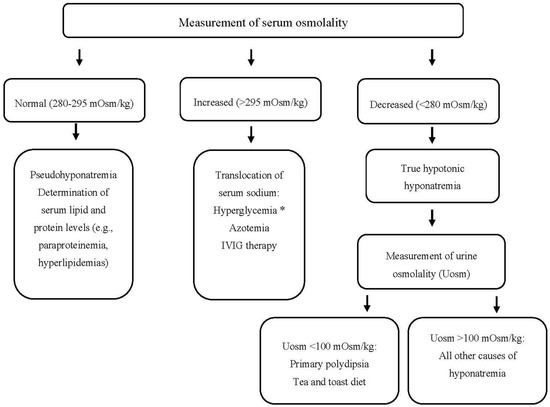
Furthermore hyponatremia and renal dysfunction are associated with poor prognosis. Hyponatremia is decrease in serum sodium concentration 136 mEqL 136 mmolL caused by an excess of water relative to solute. Common causes include diuretic use diarrhea heart failure liver disease renal disease and the syndrome of.
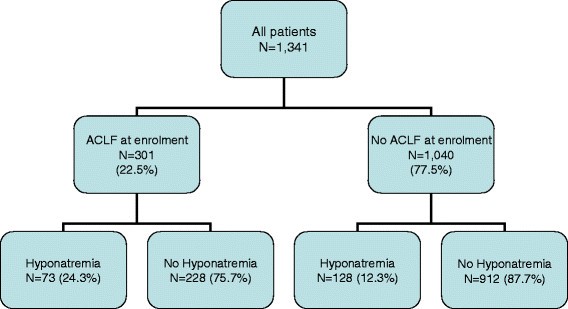
Hyponatremia is a commonly observed complication that is related to hypoalbuminemia and portal hypertension in patients with advanced liver cirrhosis. Hyponatraemia is a commonly encountered problem in patients with end-stage liver disease. However experts say that it occurs in about 57 of cirrhosis patients in hospital admission.
Hyponatremia usually occurs in the final stage of liver disease and is difficult to differentiate if the symptoms are within it or are part of liver encephalopathy occurrence. Although hyponatremia is a common electrolyte disorder encountered by physicians in clinical practice its management in the setting of advanced liver cirrhosis can be challenging. It happens in different ways and could be more severe in some people than in others.
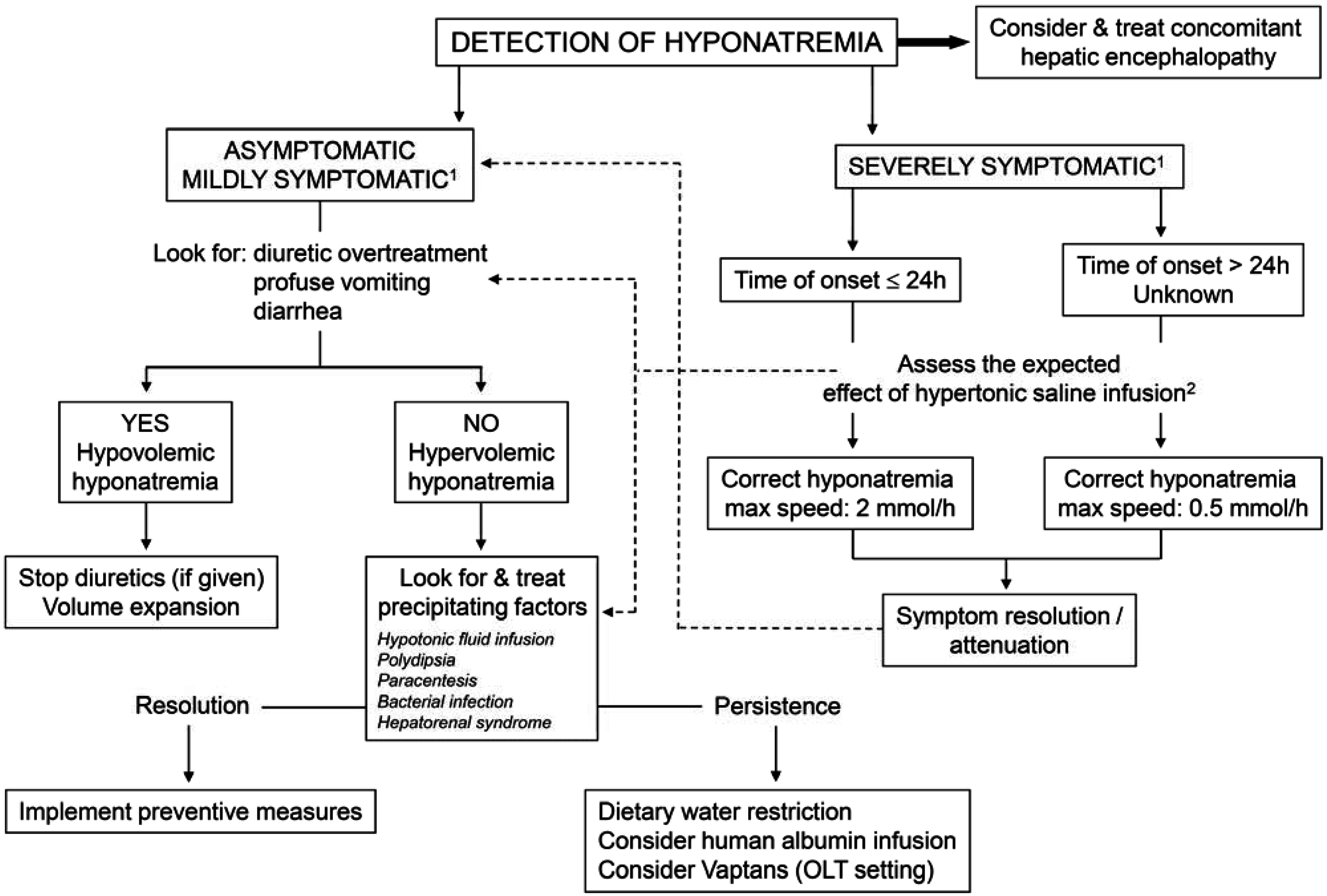
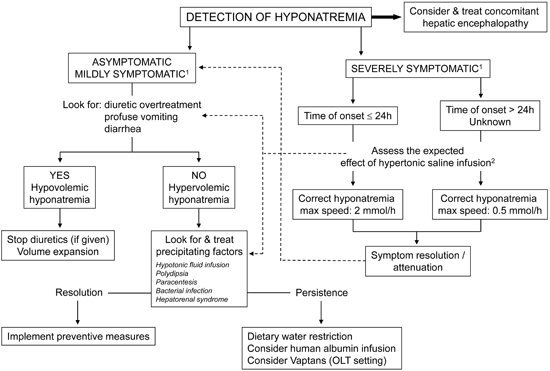
In pre-transplant patients with ESLD hyponatremia appears to be associated with manifestations of decompensated liver disease such as ascites hepatic encephalopathy and spontaneous bacterial peritonitis with these complications appearing with greater frequency in patients with more severe hyponatremia. The management of hyponatremia in this setting is a challenge as conventional therapy for hyponatremia including fluid restriction and loop diuretics are frequently inefficacious.
Hyponatraemia is a commonly encountered problem in patients with end-stage liver disease.
In patients without liver disease hyponatremia is primarily associated with a broad variety of neurological manifestations related to the existence of brain edema such as headache disorientation confusion focal neurological deficits seizures and in some cases death due to cerebral herniation. Low serum sodium is a poor prognostic indicator in both the pre- and post-transplant patient population and has been shown to increase the risk of early mortality and complications including infection renal failure and encephalopathy. The main indications for correction of hyponatremia are presence of neurologic symptoms that might be due to hyponatremia and serum sodium less than 120 mEqL. COrresPOnDenCe Bashar Attar MD PhD Division of Gastroenterology and Hepatology Cook County Health 1901 West Harrison Street Chicago IL 60612. The pathogenesis of hyponatremia in these patients is directly related to the hemodynamic changes and secondary. In pre-transplant patients with ESLD hyponatremia appears to be associated with manifestations of decompensated liver disease such as ascites hepatic encephalopathy and spontaneous bacterial peritonitis with these complications appearing with greater frequency in patients with more severe hyponatremia. The pathophysiology of hyponatremia in cirrhosis is complex and multifactorial. Liver disease About Press Copyright Contact us Creators Advertise Developers Terms Privacy Policy Safety How YouTube works Test new features 2021 Google LLC. Hyponatremia is also associated with numerous complications in liver disease patients including severe ascites hepatic encephalopathy infectious complications renal impairment increased severity of liver disease in cirrhosis and increased hospital stay and neurologicinfectious complications posttransplant.
Hyponatremia is a commonly observed complication that is related to hypoalbuminemia and portal hypertension in patients with advanced liver cirrhosis. 14 Severity of neurological symptoms in patients with hyponatremia correlates roughly with the levels of. Furthermore hyponatremia and renal dysfunction are associated with poor prognosis. The management of hyponatremia in this setting is a challenge as conventional therapy for hyponatremia including fluid restriction and loop diuretics are frequently inefficacious. Low serum sodium is a poor prognostic indicator in both the pre- and post-transplant patient population and has been shown to increase the risk of early mortality and complications including infection renal failure and encephalopathy. If the hyponatremia is persistent liver transplant evaluation should be considered. However experts say that it occurs in about 57 of cirrhosis patients in hospital admission.























Post a Comment for "Hyponatremia In Liver Disease"